Introduction
A paramedic who hasn't smiled in months. A construction foreman snapping at his crew over minor mistakes. A nurse calling in sick for the third time this week. These aren't just bad days—they're potential warning signs of a mental health crisis brewing beneath the surface of your high-stress workplace.
In industries where the stakes are high and the pressure never lets up, mental health challenges don't announce themselves with fanfare. They creep in gradually, disguised as irritability, fatigue, or declining performance. By the time most organizations recognize the signs, they're already dealing with burnout, workplace accidents, or losing valuable employees altogether.
This comprehensive guide will equip you with the knowledge to identify mental health red flags specific to high-pressure work environments like healthcare, construction, emergency services, and other demanding industries. You'll learn evidence-based screening approaches, practical intervention strategies, and how to build a workplace culture that supports mental wellness before crisis hits. Whether you're a manager noticing changes in your team, an HR professional developing support programs, or a safety officer concerned about the connection between mental health and workplace incidents, this guide provides the actionable tools you need to protect your workforce.

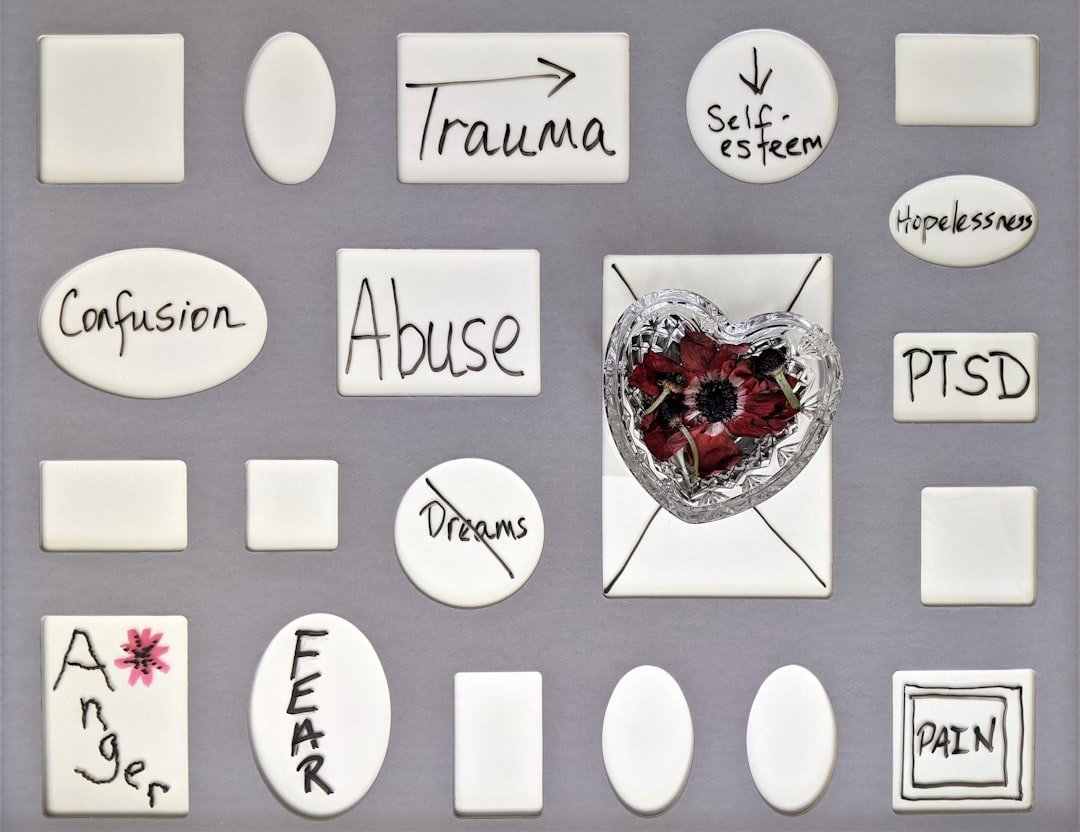
Photo by Arturo Esparza on Unsplash
What is Workplace Mental Health Safety?
Workplace mental health safety represents the systematic approach to identifying, preventing, and addressing psychological hazards in the work environment. Unlike traditional safety programs that focus on physical hazards like machinery, chemicals, or fall risks, mental health safety recognizes that psychological well-being directly impacts worker safety, productivity, and organizational success.
In high-stress industries, workplace mental health safety becomes particularly critical because the consequences of unaddressed mental health issues extend far beyond individual suffering. A distracted emergency responder, an exhausted crane operator, or a burned-out surgeon doesn't just experience personal distress—they pose potential safety risks to themselves, their coworkers, and the people they serve.
The concept encompasses several interconnected elements:
-
Recognizing psychosocial risk factors inherent to specific job roles and work environments
-
Implementing systems to identify behavioral and performance changes that signal emerging mental health concerns
-
Establishing clear pathways for addressing concerns when they're identified
-
Building resources, programs, and cultural norms that promote psychological wellness
-
Creating processes for employees to recover and successfully return to work after mental health challenges
According to the World Health Organization, depression and anxiety cost the global economy an estimated $1 trillion per year in lost productivity. However, for every dollar invested in scaled-up treatment for common mental disorders, there's a return of $4 in improved health and productivity.
Workplace mental health safety isn't about turning managers into therapists or diagnosing conditions. Instead, it's about creating an environment where early signs of distress are noticed, appropriate support is accessible, and seeking help is normalized rather than stigmatized. This approach treats mental health with the same systematic attention that organizations apply to preventing physical injuries.
Why Mental Health Red Flags Matter in High-Stress Industries
High-stress industries face a perfect storm of mental health risk factors that make early detection not just beneficial but essential for workplace safety. The nature of these jobs—whether responding to emergencies, working at heights, caring for critically ill patients, or operating heavy machinery—creates unique psychological pressures that compound over time.
The Elevated Risk Profile
Workers in high-stress industries consistently show higher rates of mental health challenges compared to the general workforce. First responders experience PTSD at rates estimated between 10-32%, compared to about 6.8% in the general population, according to research published by the Substance Abuse and Mental Health Services Administration. Healthcare workers, particularly since the COVID-19 pandemic, report burnout rates exceeding 50% in some studies. Construction workers face suicide rates nearly four times higher than the national average.
These statistics aren't just numbers—they represent real people struggling in silence, often in roles where admitting vulnerability feels impossible.
The Safety Connection
Mental health and physical safety are inextricably linked in high-stress environments. Research consistently demonstrates that workers experiencing depression, anxiety, burnout, or PTSD have:
- Impaired concentration and decision-making: Critical in environments where split-second choices determine outcomes
- Slower reaction times: Dangerous when operating machinery, responding to emergencies, or working at heights
- Increased risk-taking behavior: Sometimes manifesting as not following safety protocols or taking shortcuts
- Higher absenteeism: Leading to understaffing and overworked remaining team members
- Presenteeism: Coming to work while unwell, which can be more dangerous than absence in safety-critical roles
A study published in the Journal of Occupational and Environmental Medicine found that workers with depression had a 47% higher rate of workplace injuries compared to their non-depressed colleagues. In industries where injuries can be catastrophic or fatal, this correlation demands attention.
The Ripple Effect
When one team member struggles silently with mental health challenges, the impact extends throughout the organization:
| Impact Area | Individual Effects | Team/Organizational Effects |
|---|---|---|
| Safety | Personal injury risk, impaired judgment | Increased incidents, safety culture erosion |
| Performance | Reduced productivity, errors | Missed deadlines, quality issues, customer impact |
| Relationships | Withdrawal, conflict with coworkers | Team dysfunction, communication breakdown |
| Retention | Resignation, disability leave | Knowledge loss, recruitment costs, remaining staff burden |
| Culture | Cynicism, disengagement | Normalized unhealthy behaviors, stigma reinforcement |
Understanding why mental health red flags matter provides the foundation for taking them seriously. In high-stress industries, identifying and responding to these warning signs isn't just compassionate leadership—it's a core safety responsibility.
How to Identify Mental Health Red Flags by Industry
While certain warning signs appear across all high-stress industries, each sector presents unique manifestations based on its specific stressors, culture, and work environment. Learning to recognize industry-specific red flags helps managers and HR professionals respond more effectively.
Healthcare Industry Red Flags
Healthcare workers face the compound stress of life-and-death decisions, patient suffering, long shifts, and emotional labor. The American Nurses Association identifies healthcare as one of the most psychologically demanding professions.
-
Emotional numbness when discussing patients, cynical comments about patient care, dreading patient interactions
-
Expressions of guilt about care limitations, distress over resource allocation decisions, questioning career choice
-
Working excessive overtime without being asked, inability to leave work mentally, checking patient status from home
-
Frequent headaches, GI complaints, unexplained physical symptoms that increase around shifts
-
Avoiding break room interactions, eating alone, declining team activities they previously enjoyed
Construction Industry Red Flags
Construction workers face a unique combination of physical demands, job insecurity, seasonal work patterns, and a culture that often discourages vulnerability. The construction industry's mental health crisis has gained increasing attention from organizations like the Construction Industry Alliance for Suicide Prevention.
-
Not using PPE consistently, taking shortcuts on safety protocols, "it won't happen to me" attitudes increasing
-
Increased alcohol references, signs of impairment, using substances to manage pain or sleep
-
Conflicts with coworkers increasing, overreaction to minor frustrations, intimidating behavior
-
Chronic pain complaints, untreated injuries, fatigue-related close calls
-
Mentions of relationship problems, financial stress, housing instability common in seasonal work
Emergency Services Red Flags
First responders—including firefighters, EMTs, paramedics, and law enforcement—face repeated trauma exposure that creates cumulative psychological impact. The Code Green Campaign has been instrumental in raising awareness of mental health challenges unique to EMS professionals.
-
Inability to relax, always scanning for threats, startle responses in safe environments
-
Dark humor escalating beyond normal coping, seeming unaffected by calls that should be disturbing
-
Nightmares about calls, insomnia, excessive fatigue beyond what shift work explains
-
Requesting transfer from certain call types, avoiding locations associated with traumatic events
-
No interests outside work, relationship neglect, defining self entirely through job role
Universal Red Flags Across Industries
Regardless of industry, certain warning signs signal potential mental health concerns that warrant attention:
Behavioral Changes - Attendance pattern shifts (increased absences, arriving late, leaving early) - Performance decline in previously reliable employees - Withdrawal from team interactions and communications - Increased irritability or emotional volatility - Changes in appearance or personal hygiene
Cognitive Indicators - Difficulty concentrating or making decisions - Memory problems or forgetting procedures - Pessimistic outlook or hopeless statements - Confusion about tasks previously mastered
Physical Signs - Visible fatigue beyond normal work demands - Significant weight changes - Frequent minor illnesses - Physical complaints without clear cause
The Importance of Pattern Recognition
Individual signs in isolation may mean nothing—everyone has off days. The key is recognizing patterns: multiple signs appearing together, changes that persist over weeks rather than days, or gradual shifts from an employee's baseline behavior. Document observations objectively, focusing on observable behaviors rather than assumptions about internal states.
Implementing Effective Screening and Assessment Tools
Moving from awareness to action requires implementing systematic approaches to mental health screening. Effective assessment doesn't require managers to become diagnosticians—rather, it involves using validated tools appropriately and knowing when to connect employees with professional resources.
Organizational Assessment Approaches
Before focusing on individual screening, organizations benefit from assessing their overall mental health climate. This provides context for individual concerns and identifies systemic issues requiring attention.
-
Use validated tools like the Copenhagen Psychosocial Questionnaire (COPSOQ) or HSE Management Standards to evaluate organizational risk factors
-
Track absenteeism patterns, turnover rates, workers' compensation claims, and safety incident trends for mental health correlations
-
Anonymous surveys about stress levels, workload, support availability, and psychological safety provide valuable aggregate data
-
Aggregate (non-identifying) data from Employee Assistance Programs reveals organizational mental health trends
Individual Screening Tools for Managers
Managers are often the first to notice changes in their team members. The following approaches help structure observations and conversations:
Structured Observation Framework
Rather than relying on gut feelings, use a consistent framework for documenting concerns:
- Behavior observed: Specific, objective description of what you noticed
- Context: When, where, and circumstances surrounding the observation
- Frequency: Single instance or recurring pattern
- Baseline comparison: How does this differ from the employee's typical behavior?
- Impact: Effect on work performance, safety, or team dynamics
Conversation Starters That Open Doors
When concerns warrant a direct conversation, these evidence-based approaches create psychological safety:
The most effective question isn't 'Are you okay?'—which invites a reflexive 'I'm fine.' Instead, try 'I've noticed [specific observation]. I'm concerned about you. What's going on?' This shows you've been paying attention and creates space for honesty.
Validated Screening Instruments
Several validated tools can support mental health screening when used appropriately:
PHQ-9 (Patient Health Questionnaire-9) A nine-item depression screening tool widely used in occupational settings. Available free from PHQ Screeners. Best used by trained professionals or as part of health assessments, not for manager-administered screening.
GAD-7 (Generalized Anxiety Disorder-7) A seven-item anxiety screening tool that complements depression screening. Also available through PHQ Screeners.
PC-PTSD-5 (Primary Care PTSD Screen) A five-item screen for PTSD particularly relevant in emergency services and healthcare settings. Available from the National Center for PTSD.
Burnout Assessment Tool (BAT) Developed specifically for occupational burnout assessment, measuring exhaustion, mental distance, cognitive impairment, and emotional impairment.
| Tool | Best Used For | Administered By | Time Required |
|---|---|---|---|
| PHQ-9 | Depression screening | Healthcare provider, EAP | 3-5 minutes |
| GAD-7 | Anxiety screening | Healthcare provider, EAP | 2-3 minutes |
| PC-PTSD-5 | PTSD screening (first responders) | Healthcare provider, EAP | 1-2 minutes |
| BAT | Occupational burnout | HR/Occupational health | 10-15 minutes |
| Observation Framework | Manager-level concerns | Direct supervisors | Ongoing |
Critical Considerations for Screening Implementation
Privacy and Confidentiality Screening data is sensitive health information. Ensure compliance with HIPAA, ADA, and state privacy laws. Individual screening results should flow to qualified professionals, not HR files or personnel records.
Voluntary Participation While some industries (like transportation or public safety) have mandatory fitness-for-duty evaluations, general mental health screening should be voluntary. Coerced participation undermines trust and validity.
Cultural Competence Screening approaches must account for cultural differences in expressing distress and attitudes toward mental health. What looks like a red flag in one cultural context may be normal in another.
Follow-Through Resources Never screen without resources to respond. Identifying problems without providing solutions causes harm. Ensure EAP access, insurance coverage for mental health services, and clear referral pathways before implementing screening.
Common Mistakes to Avoid in Addressing Workplace Mental Health
Even well-intentioned mental health initiatives can backfire when organizations fall into common traps. Understanding these pitfalls helps you design more effective approaches and avoid causing unintended harm.
Mistake #1: Treating Mental Health as an Individual Problem
Many organizations respond to mental health concerns by offering individual resources—EAP counseling, stress management apps, resilience training—while ignoring systemic factors creating distress. This approach places the burden on employees to "fix themselves" rather than addressing workplace conditions contributing to the problem.
- Individual resources provide immediate support for those ready to seek help
- Apps and programs can be deployed quickly and at scale
- Respects individual autonomy and choice
- Implies the problem is employee weakness rather than workplace conditions
- Doesn't address root causes like understaffing, poor management, or unrealistic demands
- Can feel like 'wellness washing'—appearing to care without making real changes
- Employees may disengage if they see resources as performative
The Fix: Balance individual support with organizational change. When you identify mental health concerns, ask: "What about this workplace might be contributing to the problem?" Address both the individual need and the systemic issue.
Mistake #2: Waiting for Crisis to Act
Many organizations only address mental health after a tragic event—a suicide, a serious incident, or a public crisis. This reactive approach misses opportunities for prevention and signals that mental health only matters when something catastrophic happens.
The Fix: Implement proactive mental health initiatives during calm periods. Regular check-ins, ongoing training, and normalized conversations about mental health should be standard operations, not crisis responses.
Mistake #3: One-Size-Fits-All Approaches
Purchasing a corporate wellness package and deploying it uniformly across the organization ignores the reality that different roles, shifts, and demographics have different mental health needs and preferences.
The Fix: Tailor approaches to your workforce. Night shift workers need different support than day shift. Field workers need different access points than office staff. Younger workers may prefer app-based resources while others prefer in-person support. Gather input from employees about what would actually help them.
Mistake #4: Untrained Managers Attempting Intervention
Managers who recognize red flags but lack training may respond in ways that cause harm—conducting amateur therapy sessions, making promises they can't keep, sharing confidential information, or inadvertently discriminating.
The Fix: Provide Mental Health First Aid training or equivalent for all supervisors. Training should cover: recognizing signs of distress, having supportive conversations, understanding boundaries, knowing when and how to refer, and legal/ethical considerations.
Mistake #5: Creating Programs That Add Burden
Ironically, some wellness programs add to employee stress. Mandatory participation in lunchtime wellness activities, pressure to use meditation apps, or requiring detailed documentation of "self-care activities" creates additional demands on already stretched workers.
The Fix: Make support accessible but not mandatory. Reduce work demands to create time for wellness rather than adding wellness on top of existing demands. Ask employees what would actually reduce their stress rather than assuming.
Mistake #6: Stigmatizing Through Over-Concern
Sometimes organizations overreact to mental health disclosures, treating employees as fragile, removing them from challenging work, or subjecting them to excessive monitoring. This well-meaning over-concern can be as damaging as neglect.
The Fix: Respond to mental health concerns the same way you'd respond to physical health concerns—with appropriate accommodation and support while respecting the person's capability and autonomy. Follow the employee's lead on what they need.
Mistake #7: Neglecting Manager Mental Health
Front-line managers in high-stress industries face compound pressures: their own job stress plus responsibility for their team's wellbeing. Organizations often train managers to support others while ignoring that managers themselves may be struggling.
You can't pour from an empty cup. We ask supervisors to be mental health champions for their teams, but if we don't support their mental health, we're setting everyone up for failure.
The Fix: Include managers in mental health support programs. Provide peer support specifically for supervisors. Acknowledge the emotional labor of managing others and provide resources to sustain it.
Best Practices for Supporting At-Risk Employees
Once you've identified potential mental health concerns, responding effectively requires balancing compassion with professionalism, respecting boundaries while offering support, and knowing when to involve additional resources. These best practices provide a framework for supportive intervention.
Creating Psychologically Safe Conversations
The way you approach an employee about mental health concerns can either open doors or slam them shut. Research on psychological safety, pioneered by Harvard professor Amy Edmondson, shows that people only share vulnerable information when they believe they won't be punished or humiliated.
-
Private location, adequate time, not during high-stress moments or right before important deadlines
-
Start by expressing genuine concern for the person, not concern about their productivity
-
Say 'I've noticed you've been quieter in meetings lately' not 'You seem depressed'
-
Your role is to open the door and create space, not to fix or diagnose
-
Don't say 'It could be worse' or 'Look on the bright side'—just acknowledge their experience
-
Make resources available without demanding they be used. Respect their agency
Building a Tiered Response System
Effective organizations develop graduated response protocols based on concern severity:
Level 1: Monitoring and Informal Support - For mild concerns or early warning signs - Increased check-ins, informal conversations - Sharing information about available resources - Adjusting workload if possible and appropriate
Level 2: Formal Support Engagement - For persistent or moderate concerns - Formal referral to EAP - Documentation of concerns and actions taken - Consideration of temporary accommodations - Involvement of HR for guidance
Level 3: Intensive Intervention - For severe concerns or safety issues - Immediate involvement of mental health professionals - Fitness-for-duty evaluation if safety-sensitive role - Crisis resources if imminent risk - Coordinated return-to-work planning
Accommodation Strategies That Work
Under the Americans with Disabilities Act, mental health conditions that substantially limit major life activities may qualify for reasonable accommodations. Even when not legally required, accommodations can help employees remain productive while managing mental health challenges.
Effective accommodations in high-stress industries include:
Schedule Flexibility - Modified start/end times to accommodate treatment appointments - Temporary reduction in hours during acute episodes - Predictable scheduling (where possible) to support routine
Workload Adjustments - Temporary reassignment from highest-stress duties - Breaking large projects into smaller, manageable tasks - Providing additional time for task completion during recovery
Environmental Modifications - Quiet workspace for those with anxiety or concentration difficulties - Regular breaks for stress management - Reduced exposure to specific triggers where feasible
Support Enhancements - More frequent check-ins with supervisor - Peer buddy system for additional support - Written instructions to supplement verbal communication

Photo by Daoud Abismail on Unsplash
Peer Support Programs
Peer support—trained coworkers providing emotional support and practical assistance—has shown particular effectiveness in high-stress industries where professional help-seeking is stigmatized.
Successful peer support programs share common elements:
- Careful selection: Peers chosen for natural helping abilities, trustworthiness, and respect from coworkers
- Thorough training: 16-40 hours of initial training covering active listening, crisis recognition, boundaries, and self-care
- Clear scope: Peers provide support and connection to resources, not therapy or clinical intervention
- Ongoing supervision: Regular debriefing with mental health professionals to support peer supporters
- Organizational backing: Leadership support, protected time for peer support activities, and integration with formal mental health resources
The International Association of Fire Chiefs, Code Green Campaign, and other organizations provide peer support implementation guides specific to high-stress industries.
Supporting Return to Work
When employees take leave for mental health reasons, the return-to-work process significantly impacts their long-term success. Best practices include:
-
Meet with employee before return to discuss any needed accommodations, answer questions, and address concerns
-
Part-time hours or modified duties initially, increasing to full capacity over weeks
-
One person (supervisor or HR) as primary point of contact for questions and concerns
-
Brief team appropriately (respecting privacy) to ensure welcoming environment
-
Scheduled meetings during first weeks back to identify and address issues quickly
-
Recognition that recovery isn't linear and needs may fluctuate
Building a Sustainable Mental Health Safety Culture
Identifying red flags and responding to individual crises is essential but insufficient. True workplace mental health safety requires embedding psychological wellness into organizational culture—making it as fundamental as physical safety.
Leadership Commitment and Modeling
Culture change starts at the top. When leaders openly discuss mental health, share their own challenges appropriately, and prioritize wellness in decision-making, it signals that mental health matters.
Practical leadership actions include:
- Visible use of mental health resources: Leaders who mention using EAP or taking mental health days normalize help-seeking
- Incorporating mental health into safety messaging: Regular safety communications should include psychological safety alongside physical safety
- Resource allocation: Budgeting for mental health programs, training, and support demonstrates real commitment
- Policy review: Examining policies for mental health impact (scheduling, overtime, leave policies) and making changes when needed
- Accountability: Including mental health metrics in leadership performance evaluations
Integrating Mental Health into Safety Systems
Organizations with mature safety management systems can integrate mental health using existing frameworks:
Job Hazard Analysis Expansion Traditional JHAs identify physical hazards. Expand them to include psychosocial hazards: - Trauma exposure likelihood - Emotional labor demands - Work pace and workload factors - Shift work and schedule impacts - Isolation and support availability
Incident Investigation Enhancement When investigating safety incidents, include mental health factors: - Was fatigue or stress a contributing factor? - Had the involved employee shown warning signs? - Did work conditions create mental health risks? - How did organizational culture affect help-seeking?
Leading Indicator Development Track metrics that predict mental health issues before crisis: - EAP utilization trends - Sick leave patterns - Overtime hours - Turnover in specific units - Near-miss incidents potentially related to distraction or fatigue
Training at Every Level
Comprehensive mental health safety requires training tailored to different organizational roles:
All Employees - Mental health awareness basics - Recognizing distress in self and others - How to access support resources - Reducing stigma through education
Supervisors and Managers - Mental Health First Aid certification - Supportive conversation skills - Accommodation processes - Legal considerations (ADA, FMLA) - Documentation and referral procedures
HR and Safety Professionals - Advanced mental health and work training - Crisis response protocols - Program design and evaluation - Community resource navigation - Policy development for psychological safety
Senior Leadership - Strategic importance of mental health - Culture change leadership - Resource allocation decisions - Measuring and communicating ROI
Addressing Root Causes
While supporting individuals is important, sustainable mental health safety requires addressing organizational factors that create distress:
Workload Management - Realistic staffing levels based on actual demand - Clear prioritization when demands exceed capacity - Policies limiting excessive overtime - Adequate recovery time between intense work periods
Control and Autonomy - Worker input into how their work is performed - Flexibility where the job allows - Clear expectations without micromanagement - Meaningful involvement in decisions affecting their work
Social Support Infrastructure - Regular opportunities for team connection - Mentorship programs - Supervisor training in supportive leadership - Peer support programs
Recognition and Fairness - Transparent, equitable treatment - Recognition for contributions - Fair compensation and benefits - Clear pathways for growth and development
Psychological Safety - Speaking up without fear of retaliation - Mistakes treated as learning opportunities - Diverse perspectives valued - Conflict addressed constructively
Ready to Build Your Mental Health Safety Program?
Creating a comprehensive approach to workplace mental health requires understanding your organization's specific risks, resources, and culture. Start by assessing your current state and identifying the highest-priority opportunities for improvement.
Explore Our Safety Program ResourcesFAQ Section
Conclusion
Mental health red flags in high-stress industries aren't just HR concerns—they're safety signals that demand the same attention we give to physical hazards. The paramedic who hasn't smiled in months, the construction foreman whose temper has shortened, the nurse calling in sick repeatedly—these patterns tell us something important if we're willing to see it.
The evidence is clear: workplace mental health directly impacts safety outcomes, productivity, retention, and organizational success. In industries where the stakes are highest, ignoring mental health isn't just uncompassionate—it's dangerous. But the path forward isn't about turning every manager into a therapist. It's about building systems that:
- Recognize warning signs early through training and awareness
- Respond appropriately with support rather than stigma
- Refer to professional resources when individual support isn't enough
- Redesign work conditions that contribute to psychological harm
- Reinforce a culture where mental health matters as much as physical safety
The most effective workplace mental health safety programs balance individual support with organizational change. They provide resources for struggling employees while also examining and improving the conditions that contribute to distress. They train managers to have supportive conversations while also holding leadership accountable for creating psychologically healthy workplaces.
As you move forward from this guide, consider starting with these concrete next steps:
- Assess your current state: Use the organizational assessment approaches described to understand your starting point
- Train your supervisors: Equip front-line managers with skills to recognize and respond to mental health concerns
- Review your resources: Ensure EAP and other support resources are accessible, known, and adequate
- Examine your culture: Honestly evaluate whether your workplace culture supports or undermines mental health
- Track and measure: Begin collecting data on mental health indicators so you can monitor progress
Every worker in every high-stress industry deserves to come home from work not just physically safe, but psychologically whole. Making that happen requires commitment, resources, and sustained attention—but the evidence shows it's both achievable and worthwhile. The organizations that recognize mental health as a core safety issue will be the ones that retain their best people, prevent tragic incidents, and build workplaces where people can thrive even under pressure.
The warning signs are there. The question is whether we choose to see them—and what we do when we do.
Karen Mitchell is the Senior Safety Editor at the Academy of Occupational Health & Risk Sciences. With over 15 years of experience in occupational health and safety, she specializes in translating complex workplace safety requirements into practical guidance for safety professionals, HR managers, and organizational leaders.
Comments
No comments yet. Be the first to comment!
Leave a Comment